PEOPLE ON THE CHIP
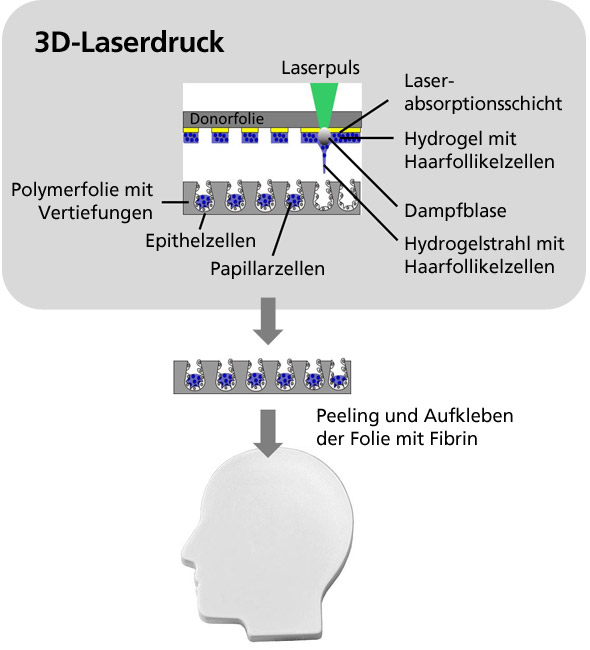
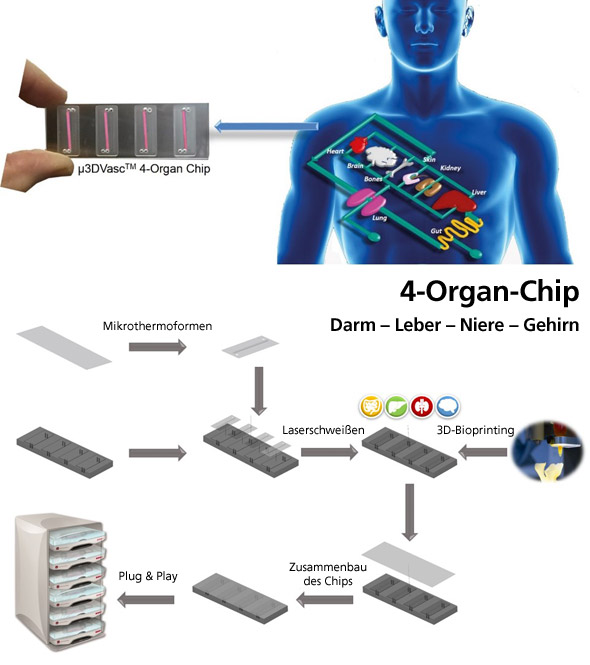
Drug testing on humans repeatedly results in adverse health effects, sometimes even fatal. Animal experiments, on the other hand, are ethically questionable and their results are not always transferable to the human body. Miniaturized human 3D tissues and organs made from different cells, so-called body-on-a-chip, can already provide indications of of drug tolerability in humans in the preclinical phase, thus minimizing the risk in the clinical phases. There is a need for in vitro systems in which supplying blood vessels can be grown in combination with 3D tissues and which meet the physical and mechanical demands of a blood vessel system. Today, there are few microfluidic chip systems, which however consist of angular channels and do not represent the curved environment of a blood vessel or the flow profile of the blood vessel. Prof. Schepers' research group was able to develop a three-dimensional microfluidic blood vessel system consisting of round, porous and branched channels through microthermoforming, onto which miniaturized 3D organs can be 3D bioprinted from human cells. Resulting low-cost disposable products can reduce the cost of pharmaceutical research and minimize the number of animal experiments.
WITH LIGHT AGAINST CANCER
Despite advances in cancer treatment, there are still problems with many chemotherapeutics, such as drug resistance or serious side effects due to the simultaneous killing of stem cells and proliferating tissue. Likewise, it remains a challenge with radiation therapy to avoid damaging surrounding healthy tissue. Photodynamic therapy is an innovative treatment method for cancer based on light-inducible active substances, so-called photosensitizers. The photosensitizer is injected into the patient’s bloodstream and is initially completely harmless to the body. Only when irradiated with light of a certain wavelength does the photosensitizer develop its toxic effect: Local exposure of the tumour results in the formation of reactive oxygen species that destroy the tumors.
However, conventional photosensitizers such as titanium dioxide are not suitable for the treatment of deep-lying tumors, as they are activated with UV light, which has a low penetration depth in the human body and is cell damaging. Photosensitizers, which are activated with longer-wave light, are therefore of great interest for tumor therapy. The research group has developed light-sensitive β-tin tungstate nanoparticles, which, in contrast, are very stable under physiological conditions. Since they are activated with visible light, deeper tumors can also be treated.
FLUORENSCENT SPRAY AGAINST MELANOMA
Malignant melanoma, the black skin cancer, is one of the most dangerous types of skin cancer. If detected in the advanced stage, there is little chance of recovery. If a malignant melanoma is detected early, there is a good chance of recovery. Early detection is mainly performed by surgical removal and histological examination of degenerated liver patches. This method is complex and allows only random examinations of patients.
One of Prof. Scheper’s product ideas is based on the development of a contact gel or a spray for the whole body treatment and the subsequent detection of degenerated skin areas using a commercially available and inexpensive UV lamp that stimulates the fluorescence of the dye and makes the degenerated liver spots visible. Any unintaken substance can be removed by washing it off beforehand. The idea is based on a fluorescent substance synthesized by the research group, which is selectively absorbed only by cells of the malignant melanoma. Screens on human cells do not show uptake in healthy skin cells or in other cells or tumors.